World Health Organization (WHO), the leading global authority in the fight against COVID-19, has maintained that masks wearing for otherwise healthy people is unnecessary.
“Medical masks should be reserved for healthcare workers… “The use of medical masks in the community may create a false sense of security,” WHO said in a recent report that sounds internally contradictory.
WHO argues that using masks, without adopting other essential measures to protect against COVID-19 such as, physical distancing and hand hygiene, may turn around and burden our healthcare system as people may end up getting sick after touching their faces under the masks.
According to the report released April 6, WHO insisted use of mask should be restricted because masks alone, are insufficient to provide an adequate level of protection against COVID-19, and other measures should also be adopted.
This is a confusing directive. It assumes members of the public, who adopt wearing masks, would stop taking other measures. Masks work as a preventative measure against coronavirus, otherwise, they would not be recommended for use by healthcare workers. Why not recommend wearing masks by all citizens and request them to allow healthcare workers to have them first because of their role in this fight against COVID-19?
Instead of encouraging people to take all measures, go above and beyond, to protect themselves and stop the spread of the novel coronavirus, WHO appears to be advising people to hold back.
This is a disheartening attitude, especially coming from a respected global health organization such as WHO. In wearing masks, people are emulating, a best practice credited for stopping the coronavirus from spreading in Hong Kong. George Gao, head of the Chinese Center of Disease Control, who treated COVID-19 patients in the Chinese outbreak, came out in favor of the public wearing masks.
“The big mistake in the U.S. and Europe, in my opinion, is that people aren’t wearing masks,” Gao said in a report by Science Magazine. “This virus is transmitted by droplets and close contact. Droplets play a very important role—you’ve got to wear a mask, because when you speak, there are always droplets coming out of your mouth. Many people have asymptomatic or pre-symptomatic infections. If they are wearing face masks, it can prevent droplets that carry the virus from escaping and infecting others.”
“The big mistake in the U.S. and Europe, in my opinion, is that people aren’t wearing masks.” –george Gao, head of china cdc.
In their well-intended attempt to protect health care workers from a worsening shortage of masks, WHO may have sent the wrong signal to the public that could lead to more infections. Just like it’s useless to wash your hands and fail to keep your distance, recommending other mitigation efforts over wearing masks in public sounds duplicitous.
Medicine practice is based on accepted theories. In fact, medicine, as we understand it now, has come a long way and is quite dynamic. Practices that were hailed as life-saving in one era, usually sound like old-wife’s tales when revisited decades later.
There are too many unknown factors in treating COVID-19 and WHO taking an ambivalent position toward the public wearing masks as a coronavirus preventative measure is ill-advised. All throughout history, we have seen great medical advancements germinate from simple best practices.
HISTORICAL METHODS OF MEDICAL PRACTICE
There is historical evidence that appendectomies were being performed well before the invention of anesthesia. To conduct the excruciatingly painful operation, they pinned patients down by strong hands to ensure they stayed still and went through the surgery.
Technology and innovation in the medical field have led to less painful innovations to perform such surgeries.
Smoking is another area that has undergone a dramatic evolution as more research about the dangers of second-hand smoke have emerged. It is not long ago that cigarette smoking was allowed in public places including hospitals, even doctors smoked cigarettes while attending their patients. Patients were allowed to smoke cigarettes in the hospital rooms, before evidence started linking the increased risk factors of cigarette smoking to high incidences of lung cancer.
There is a myriad example of the ever-changing landscape of Medicine and its practices. COVID-19 is one more example of medicine practice on the go. Nobody has a definitive treatment modality at present. We can safely say, it is a combination of anecdotal evidence and the limited science about the virus that is guiding treatment plans across the globe. The results are mixed and no conclusive treatment plans yet.
It is in this darkness that an information cesspool has emerged. There are many treatments, best practices and general disease processes shared every second via numerous platforms. This is overwhelming for consumers, leaving most with a mixture of emotions ranging from depression, anxiety, curiosity or straight up indifference.
The virus has exposed the truth about medicine, that it is, perhaps, really a practice of informed guesswork. That you must have the background details of a condition, but when it gets down to it, making a diagnosis and treatment it is a matter of doctors making their best guess.
We must realize that we are in this together and take all precautions. It is better to overdo it and be healthy, than to get infected because you followed directions from WHO that downplayed the benefits of wearing medical masks or face covering.
We are all struggling to find a solution to an unpleasant surprise. But the question persists, when this is over, will we emerge more knowledgeable or more confused about COVID-19?
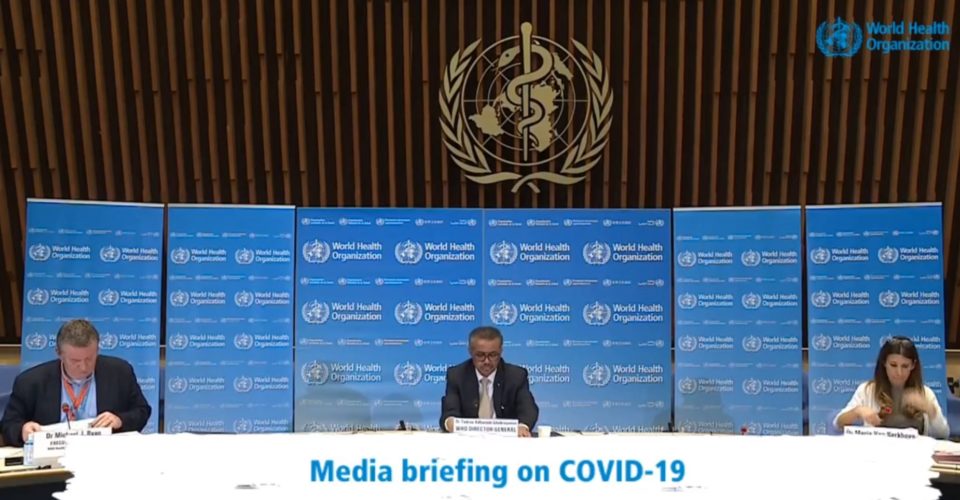
EDITOR’S UPDATE: In a 4/13/2020 press briefing, WHO supports use of masks or face-covering along with other mitigating methods such as social distancing and hand washing as part of a comprehensive approach, as long as it does not take masks away from healthcare workers.